Calcium & Vitamin D ( 600 mg Calcium ) Halal Gelatin Free Tablets
$14.99
Calcium and vitamin D work together to protect bones—calcium helps build and maintain bones, while vitamin D helps your body effectively absorb calcium. So even if one is taking in enough calcium, it could be going to waste if you’re deficient in vitamin D. Balancing both is important.
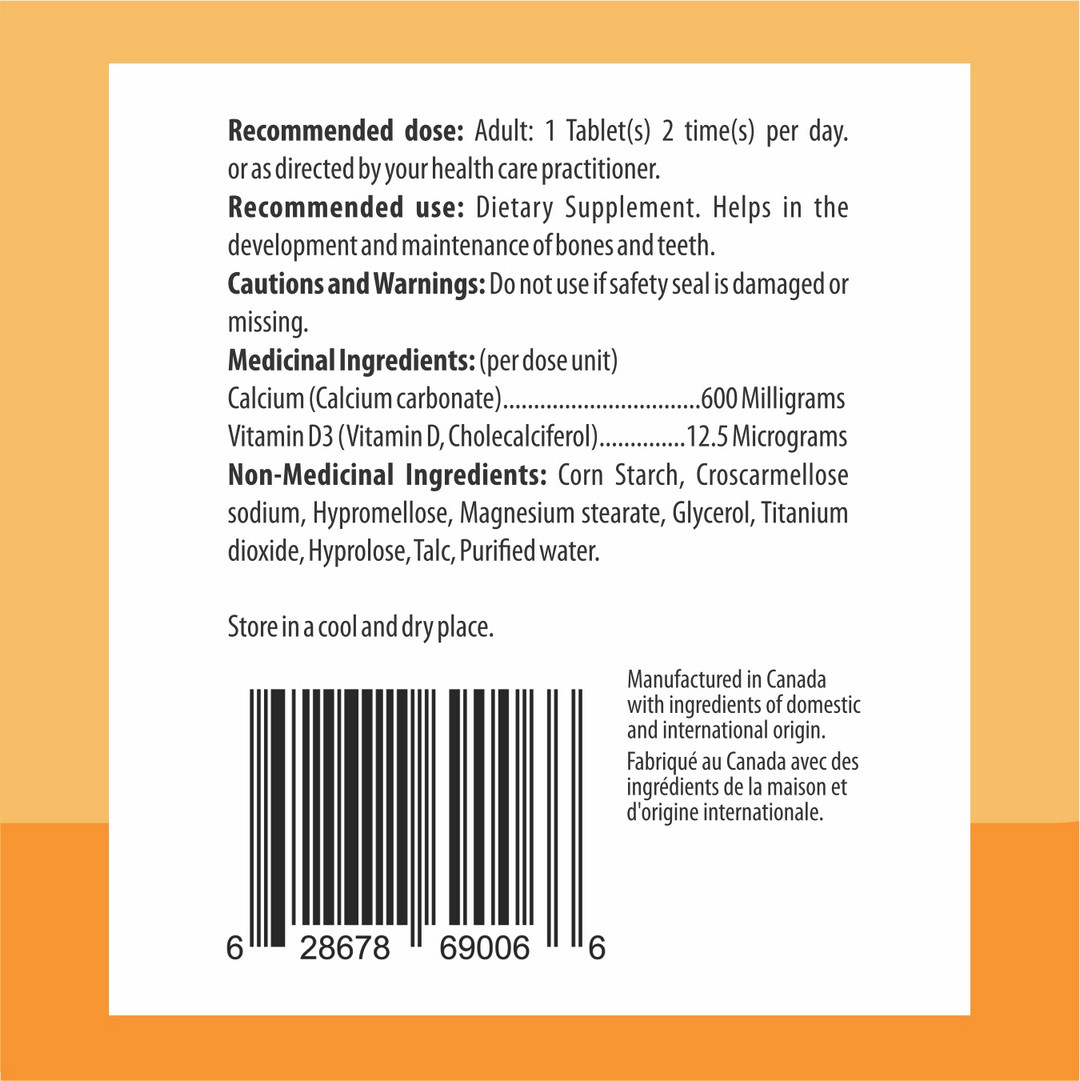
Recommended dose: Adult: 1 Tablet(s) 2 time(s) per day. or as directed by your health care practitioner.
Recommended use: Dietary Supplement. Helps in the development and maintenance of bones and teeth.

Buy 1 & Get 1 Free
Description
What is Calcium and Vitamin D?
Calcium is good for bones and helps ward off osteoporosis. The nutrient is essentially a building block of bone, and it helps maintain bone strength throughout lifetime. Calcium can only reach its full bone-building potential if your body has enough vitamin D. Without enough vitamin D or calcium, your parathyroid glands compensate by producing too much of their hormone, a condition called HYPERPARATHYROIDISM That can lead to bone weakening OSTEOPOROSIS and increased fracture risk.
Other problems from calcium and vitamin D deficiencies include:
- Skeletal deformities (rickets) in children ages 6-24 months
- Muscle weakness in children and the elderly (vitamin D only)
Given the crucial role of both nutrients in bone health, The Endocrine Society and the Institute of Medicine recommend certain consumption levels based on age and health. They have not yet found, however, that taking vitamin D provides cardiovascular protection.
HEALTH BENEFIT OF CALCIUM AND VIRAMIN D (SUMMARY)
Vitamin D (a hormone) and calcium (a mineral) are nutrients that sustain healthy bones. They are also needed for:
- Muscle movement
Specifically, vitamin D with calcium, compared to calcium alone, improved body sway by 9% in ambulatory elderly women with serum 25(OH)D levels <50 nmol/L within 8 weeks [60] and improved lower extremity muscle performance in institutionalized elders with serum 25(OH)D levels <50 nmol/L by 4-11% within 12 weeks. Similarly, in a recent longer-term study among healthy older men and women with serum 25(OH)D levels <75 nmol/L, vitamin D3 800 IU and calcium 1000 mg daily, compared to calcium alone, significantly improved tests of physical performance over a 12-20-month period. A randomized trial in 179 pre-menarchal girls, age 10-17, who received either oral vitamin D3 1,400 IU/week, vitamin D3 14,000 IU/week or placebo for 1 year, reported an increase in whole body lean mass (a surrogate marker of muscle mass) in supplemented girls
- Nerve communication
One important yet little known of the numerous functions of vitamin D is the regulation of nervous system development and function. The neuroprotective effect of vitamin D is associated with its influence on neurotrophic production and release, neuromodulator synthesis, intracellular calcium homeostasis, and prevention of oxidative damage to nervous tissue. Clinical studies suggest that vitamin D deficiency may lead to an increased risk of disease of the central nervous system (CNS), particularly schizophrenia and multiple sclerosis. Adequate intake of vitamin D during pregnancy and the neonatal period seems to be crucial in terms of prevention of these diseases.
- Absorption of calcium and phosphorous (vitamin D)
The main function of vitamin D is to maintain calcium (Ca) and phosphorus (P) balance in the body by promoting Ca and P absorption from the intestines and kidneys (5). In vitamin D deficiency, only 10%-15% of calcium and 50%-60% of phosphorus can be absorbed from ingested foods. Vitamin D functions by stimulating intestinal calcium and phosphorus absorption, by stimulating bone calcium mobilization, and by increasing renal reabsorption of calcium in the distal tubule. These functions on bone and possibly kidney, but not intestine, require the parathyroid hormone. As a result of these functions, serum calcium and phosphorus concentrations are elevated to supersaturating levels required for the mineralization of bone to prevent rickets, osteomalacia, and hypocalcemic tetany. Recent experiments demonstrate that maintaining serum calcium and phosphorus levels in vitamin D-deficient rats in the normal range results in normal bone growth and mineralization.
- Immune system responses (vitamin D)
Vitamin D has important functions beyond those of calcium and bone homeostasis which include modulation of the innate and adaptive immune responses. Vitamin D deficiency is prevalent in autoimmune disease. Cells of the immune system are capable of synthesizing and responding to vitamin D. Immune cells in autoimmune diseases are responsive to the ameliorative effects of vitamin D suggesting that the beneficial effects of supplementing vitamin D deficient individuals with autoimmune disease may extend beyond effects on bone and calcium homeostasis.
- Signaling between cells (calcium)
Vitamin D is a hormone that maintains healthy cells. It functions by regulating the low resting levels of cell signaling components such as Ca2+ and reactive oxygen species (ROS). Its role in maintaining phenotypic stability of these signaling pathways depends on the ability of vitamin D to control the expression of those components that act to reduce the levels of both Ca2+ and ROS. This regulatory role of vitamin D is supported by both Klotho and Nrf2. A decline in the vitamin D/Klotho/Nrf2 regulatory network may enhance the ageing process, and this is well illustrated by the age-related decline in cognition in rats that can be reversed by administering vitamin D. A deficiency in vitamin D has also been linked to two of the major diseases in man: heart disease and Alzheimer’s disease (AD). In cardiac cells, this deficiency alters the Ca2+ transients to activate the gene transcriptional events leading to cardiac hypertrophy and the failing heart.
- Hormonal secretion (calcium)
Vitamin D and its’ metabolites are a crucial part of the endocrine system that controls whole body calcium homeostasis. The goal of this hormonal control is to regulate serum calcium levels so that they are maintained within a very narrow range. To achieve this goal, regulatory events occur in coordination at multiple tissues, e.g. the intestine, kidney, bone, and parathyroid gland. Production of the vitamin D endocrine hormone, 1,25 dihydroxy vitamin D (1,25(OH)2 D) is regulated by habitual dietary calcium intake and physiologic states like growth, aging, and the menopause. The molecular actions of 1,25(OH)2 D on calcium regulating target tissues are mediated predominantly by transcription controlled by the vitamin D receptor. The primary role for 1,25(OH)2 D during growth is to increase intestinal calcium absorption so that sufficient calcium is available for bone mineralization. However, vitamin D also has specific actions on kidney and bone.
- Blood vessel flow (calcium)
Coronary artery calcified plaque is a marker for atheromatous plaque burden and predicts future risk of cardiovascular events. The relationship between calcium plus vitamin D supplementation and coronary artery calcium (CAC) has not been previously assessed in a randomized trial setting. We compared coronary artery calcium scores among women randomized to calcium/vitamin D supplementation versus placebo following trial completion.